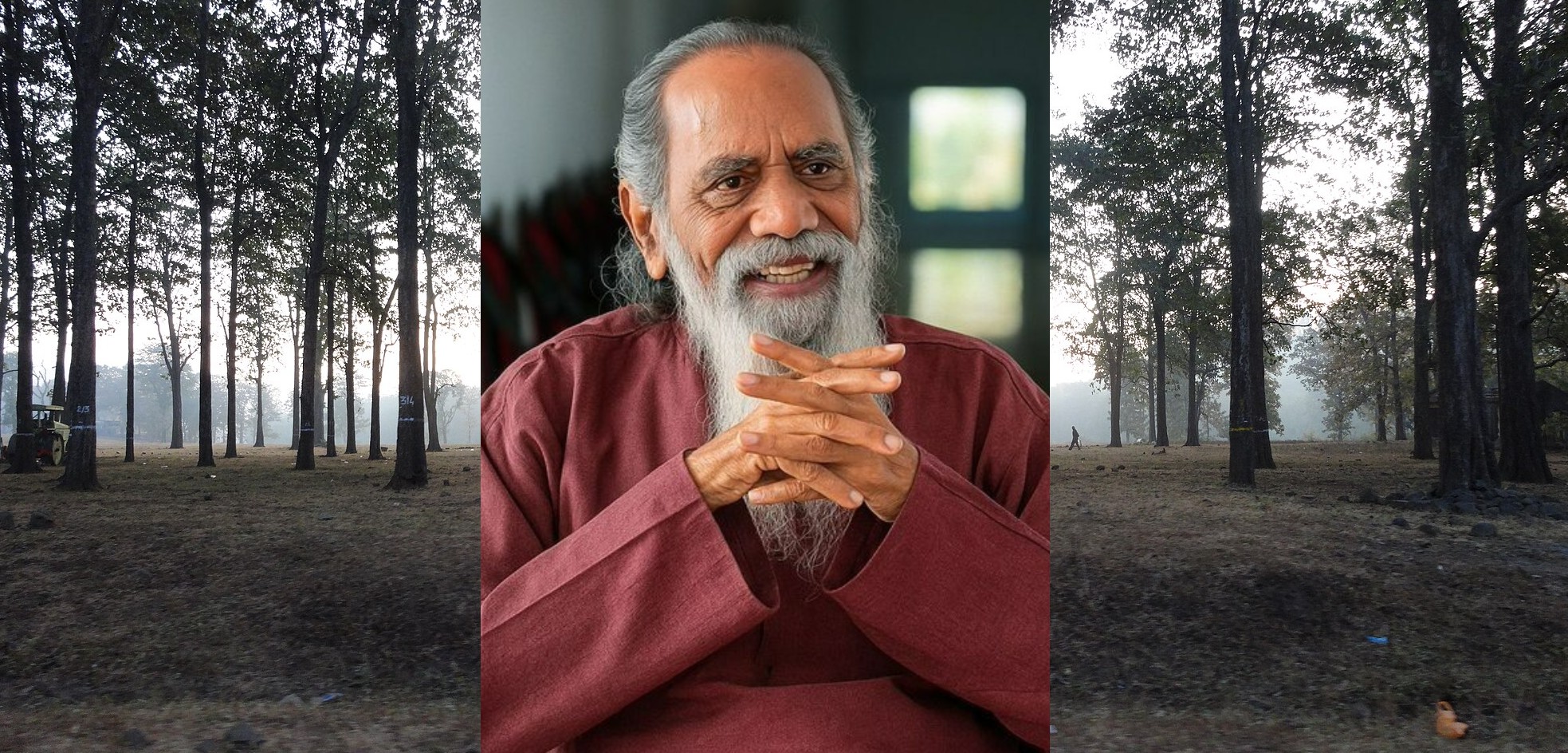
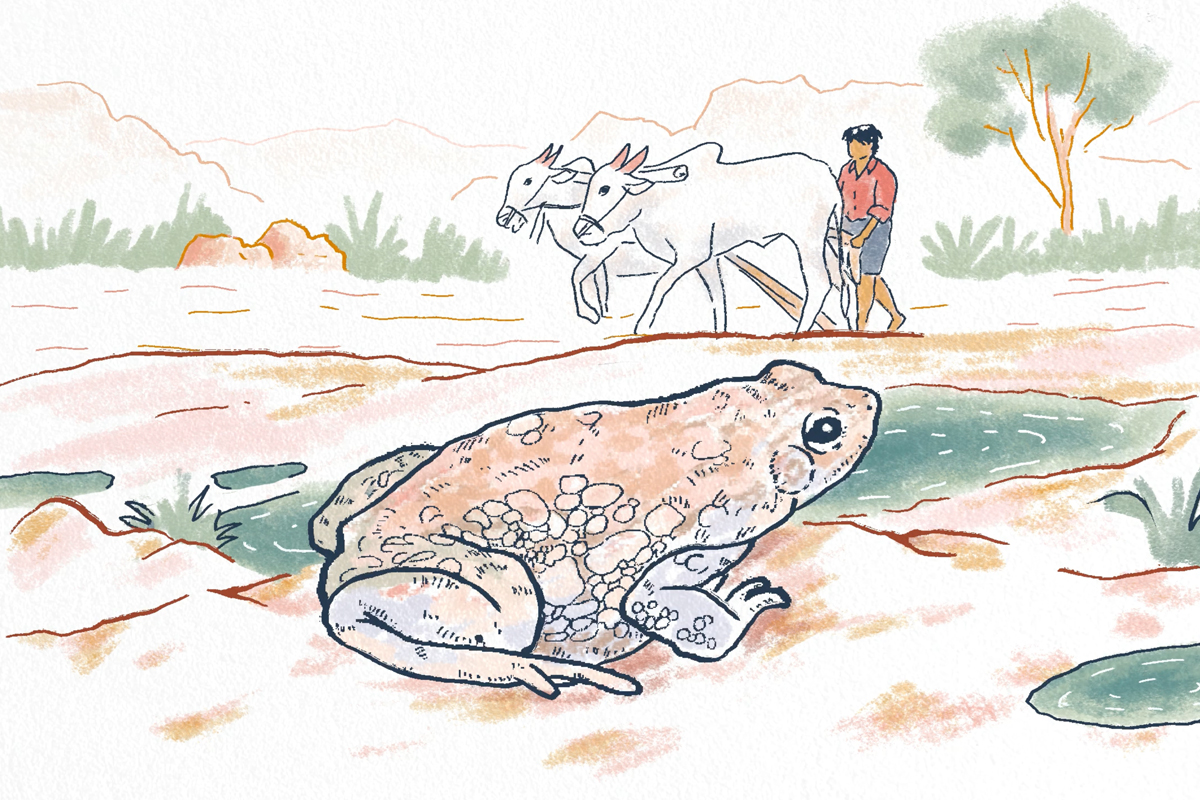
- Last year, Devi Prasad Ahirwar, a former security guard, collapsed from a heat stroke in Delhi, during one of the country’s worst episodes of extreme heat.
- While he survived, a year later, the severity of his heat stroke has resulted in rare neurological side-effects.
- The extent of neurological deficits among heatstroke survivors is not well known, but deserves closer study, doctors say.
- Emergency cooling is one of the most effective methods to reduce severe illness and mortality from heat stroke, and needs more support.
The death toll from extreme heat events always makes the headlines. But what happens when you’re on the brink of joining that number, and are brought back from the edge?
Devi Prasad Ahirwar, a 55 year-old former security guard, collapsed from a heat stroke in Delhi last year during one of the country’s worst and most prolonged episodes of extreme heat. Unconscious, with a dangerously high fever, he spent six days on a ventilator before miraculously gaining consciousness. He’d survived despite the odds, experts said.
A year later, however, the heat stroke isn’t entirely behind him. Survival gave Devi Prasad a second chance at life, but it’s a life marred by strange new afflictions his family is learning to live with. The severity of his heat stroke has resulted in rare neurological side-effects – he can no longer speak clearly, write, or get up from the floor without feeling dizzy. To walk, he now uses the help of a stick when in the past, he could walk for kilometres on end without tiring.
He now spends his days mostly silent and resting, or walking up and down the courtyard outside his village home. “He was a healthy man before he collapsed,” said Binodi Ahirwar, his wife. “It’s been a year of taking him to doctors, doing scans. When will he get better?”
The long-term neurological and physiological impacts of heat stroke are not well-studied among survivors in India, even though research points to the existence of debilitating residual effects. Though rare, Devi Prasad’s case isn’t the only one, Mongabay India found.
An incomplete recovery
When the body’s internal temperature breaches 41° Celsius (105.8 ° Fahrenheit ) it can cause cellular breakdown and multi-organ failure if left untreated. In such cases, the central nervous system is especially susceptible to damage.
“A heat stroke can cause direct injury to the brain because at high internal temperatures, the electrical activity of nerve cells is affected,” explained Atri Chatterjee, assistant professor of neurology at Vardhaman Mahavir Medical College and Safdarjung Hospital. “Unlike most other neurological disorders, a heat stroke can affect the entire brain at once, though certain parts of the brain, like the cerebellum, are more sensitive to heat.”
In the months following his heat stroke, Devi Prasad gradually regained his strength and was able to walk, take himself to the bathroom, and eat. But he never regained his speech, and his gait is unsteady. In conversation, he can comprehend, but not contribute. When he opens his mouth to say something, the words are distorted, and his family struggles to interpret.
No longer fit to resume guard duties, he returned to his village in Tikamgarh, a drought-prone district in Madhya Pradesh where outmigration is rampant. From the cramped quarters of his room in New Delhi, Devi Prasad and his wife now live in the cramped quarters of their village, with a single tree for shade. “It can become hot here too, especially when the electricity goes,” said Roshani, Devi Prasad’s daughter, who is a street vendor selling samosas.

Three weeks ago, as she fried samosas over hot oil under a relentless sun, she began to feel dizzy. “My husband and I were terrified after seeing what happened with my father,” she said, adding, “I sat myself in front of the cooler immediately. I didn’t want to risk landing up in the same situation.”
To seek a solution to his father’s problem, Devi Prasad’s eldest son, Sanjay, a construction worker, has ferried his father from doctor to doctor across three cities – Delhi, Bhopal, and Gwalior – collecting a growing pile of papers and prescriptions, all paid for by dwindling savings. But none of them carry a cure. The recommended treatment – speech and physiotherapy – is difficult to come by in Tikamgarh.
An MRI scan revealed chronic small-vessel ischemic changes in his brain, a condition that can result in restricted blood flow to the brain and, depending on the severity, cause problems with cognition, speech, and movement. In the absence of a clear case history, however, directly attributing this condition to a heat stroke is challenging. “The doctors have asked us to do the MRI scan again to check his brain, but it costs so much money. We haven’t been able to do it,” said Binodi.
Outside his immediate family, Devi Prasad’s story doesn’t serve as much of a cautionary tale, said Neha Ahirwar, a neighbour who recently completed her training as a nurse. “People don’t really understand the severity of heat stroke here. No one thinks it will happen to them.” And even if they do, they have no option but to work.
When heat stroke impairs the central nervous system
Symptoms such as slurred speech and poor coordination in the aftermath of a heat stroke are consistent with damage to the cerebellum, several doctors told Mongabay India. Located at the base of the brain, the cerebellum controls balance, posture, and coordination, and hosts a large number of Purkinje cells. These unique neurons play a fundamental role in motor movement, but are easily damaged when exposed to high temperatures.

“Damage to the cerebellum due to heat stroke can lead to the appearance of people being very unsteady, and could lead to permanent disorders of coordination, walking, and other activities. But this depends on the individual, and the consequences will depend on which other parts of the brain might have been affected,” said Sanjay Sisodiya, Professor at the UCL Queen Square Institute of Neurology and an expert on the links between climate change and neurological disorders.
A little-known research paper published by doctors in Ram Manohar Lohia Hospital, a public hospital in Delhi, recorded similar cases of persistent neurological deficits in heat stroke patients leaving the Intensive Care Unit (ICU). Like Devi Prasad, these were patients trapped in the grips of last year’s heat wave, when temperatures stayed above 41°C.
Take the case of a 38-year-old man with no known comorbidities, who was admitted into the ICU with an internal temperature of 108 degrees. After two days of treatment, his condition improved, “however, he continued to have residual neurological abnormalities, such as agitated behavior and hallucinations, and was not able to vocalize, though he was able to follow simple verbal commands,” says the paper. One month after being discharged, the patient’s behavioural changes and hallucinations had resolved, but “the deficit in spoken speech was persistent.”
The paper details two other cases in which patients were left with a combination of residual effects — one 50-year-old labourer was left after treatment with decreased verbal output and impaired comprehension, and another 67-year-old man with schizophrenia who suffered a “deficit in motor response, comprehension of spoken words, and verbal output,” one month after discharge.
Who is likely to make a full recovery and who isn’t is difficult to say, but deserves closer study, said Chatterjee. “We might typically expect to see such long-term effects in children and older populations. But we don’t have the data to really understand which populations are likely to have residual neurological impacts from heat stroke,” said Chatterjee, adding “I haven’t come across a study that tries to systematically capture the long-term impact of heat stroke on the nervous system, or any other system, on a population level.”

Mortality from heat stroke can be as high as 64%, and those suffering from long-term impacts are likely to make up a small proportion of survivors. The concern, however, is that if left unaddressed, these disabilities could become more systemic as heat waves worsen, damaging the health of those affected by rising temperatures and leaving them with conditions that are otherwise preventable.
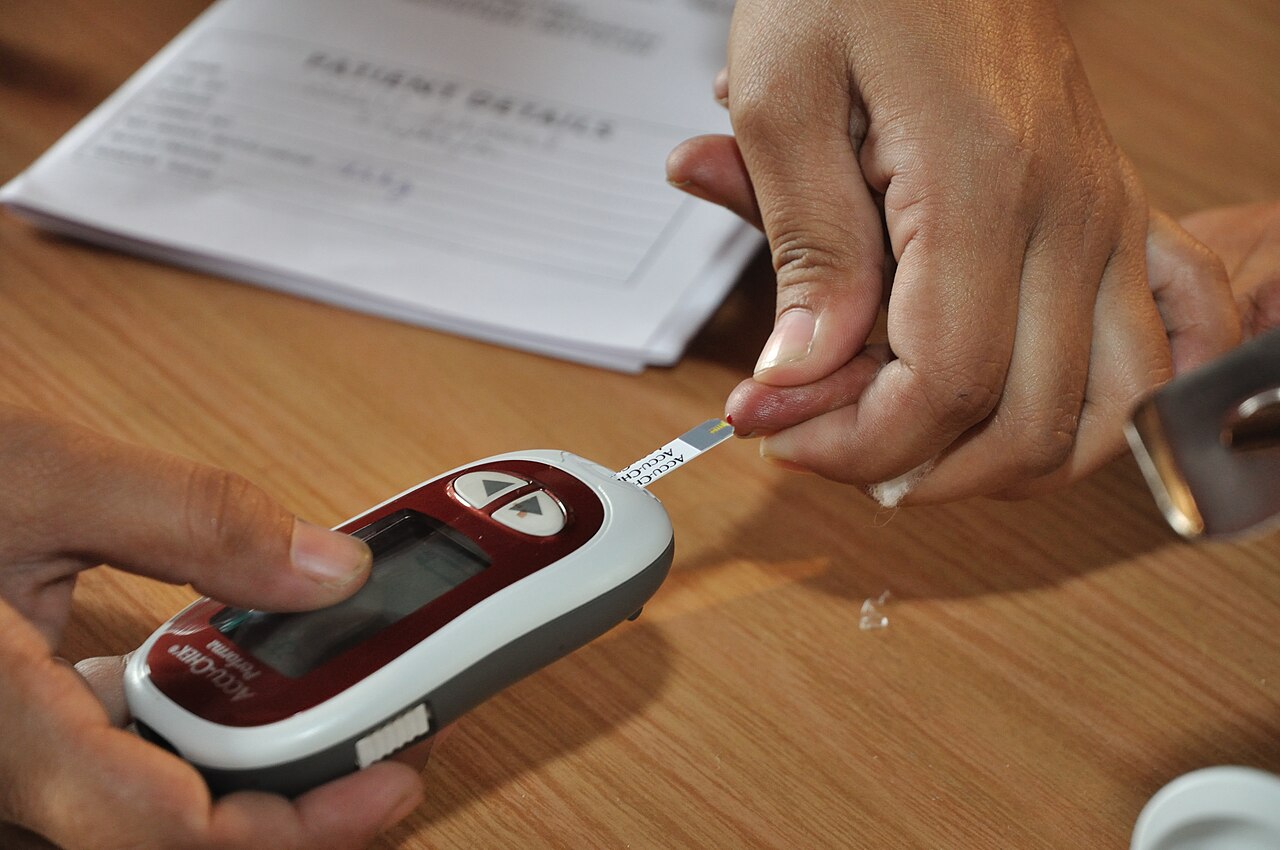
An older investigation from 2012, when parts of Chennai in Tamil Nadu were gripped by a heat wave, found that 4 out of 17 patients admitted in the ICU were discharged with neurological deficits. Most patients in the study had comorbidities like hypertension and diabetes, with an average age of 53.
“We do not have long term follow up data of our patients, but 24% had neurological deficits at hospital discharge, while other organ functions recovered,” said M.S. Kalaiselvan, a critical care specialist who authored the study. “Literature review shows neurological deficit up to 33% among survivors. We should make efforts to stop these things early, identify vulnerable populations and provide adequate education.”
The importance of emergency cooling
The biggest life saving factor involved with heat stroke is emergency cooling. “Emergency cooling can prevent patients with heat related illness from ever having to visit the ICU in the first place,” said Ajay Chauhan, a faculty of the medicine department at RML hospital, who helped set up Delhi’s first heart ward.
Emergency cooling entails rapidly bringing the body’s temperature down within 30 minutes of a serious heat related event. Guidelines issued before last year’s heat wave recommend using any materials available – cold water or ice – to cool the entire body. Ice immersion is the most efficient method, but using ice packs and cold water can work too. “Delay in cooling is directly associated with adverse outcomes including high mortality,” say the guidelines.
But a survey on the levels of heat preparedness among healthcare facilities paints a bleak picture. Of 5,690 healthcare facilities assessed across India – including primary, community, and tertiary centres – only a third had emergency cooling management practices in place, the survey, conducted by the National Programme on Climate Change and Human Health between April and June 2024, found.

Only 6% of healthcare facilities were found to have an “optimal” level of preparedness for active cooling. And 51% were found to have inadequate preparedness “for their level,” the survey said.
The onus of carrying out emergency cooling and heat stroke prevention can’t lie with health facilities alone, especially when heat stroke can occur at places of work, said Vidhya Venugopal, Professor of Occupational and Environmental Health at Sri Ramachandra Institute of Higher Education and Research.
Without a law guaranteeing rights or insurance to fall back on, migrant labourers are among the groups most likely to suffer on account of extreme heat – both economically and physiologically. Out of 75 heat stroke patients admitted in RML’s emergency heat ward, an overwhelming majority were men who worked as street vendors, labourers, and in other occupations in the unorganised sector.
“It needs to be mandatory for employers, even contractors and subcontractors, to educate their workers about the dangers of heat stroke, how to identify signs, and carry out first aid. This type of awareness is completely lacking on the ground,” said Venugopal, who is also the Country Director of the National Institute for Health and Care Research’s Centre on Environmental Change and NCDs. “Even if someone presents with a high fever and dehydration, they might be given paracetamol and sent home. The real solution lies in reducing exposure, by managing workload and heat.”
Heat Action Plans (HAPs), which are the foremost blueprints that state governments and districts use to mitigate the impacts of extreme heat, generally perform poorly when it comes to identifying and targeting vulnerable populations. For prevention measures to be more meaningful, policy must catch up.
“What we don’t know is which individuals might have individual vulnerability factors, and what the mechanisms are that link the changes in the environment to changing patterns of disease, prevalence, incidence, severity and so on,” said Sisodiya of UCL, adding, “That’s where we need more research. Unless we understand those mechanisms, all we can offer is generic support.”
Life in a hotter climate
The heat wave that sent Devi Prasad and hundreds like him to the hospital was made approximately 1.5°C hotter due to global warming, a rapid analysis found. The Ministry of Health suspects India saw 48,156 cases of heat stroke last year, nearly 40% of which were admitted in healthcare facilities, indicating serious illness.
Heatwaves are projected to become more frequent as climate change accelerates, depending on the extent of global warming. Heat waves in India are already longer by three days compared to 30 years ago.
But both the number of heat wave cases and the death count – suspected to be 269 and confirmed to be 161 — are widely accepted to be gross undercounts. Without an accurate number, determining the scale of the problem becomes a challenge, experts have argued.

A decadal analysis of all-cause mortality data by researchers from India, Sweden, and the U.S. project the number of deaths due to heat stroke in India to be 1,116 annually. In their observation, when extreme temperatures above the 97th annual percentile stay high for two days consecutively, it is associated with a 14.7% increase in daily mortality.
After a year in recovery, such hostilities in the climate are no longer a hindrance to Devi Prasad’s plans. In the absence of a cure, with no arable land to speak of, and in need of money, Devi Prasad is determined to rejoin the workforce. “The contractors who gave him the job simply ran away when he collapsed last year. We’re going to try and demand that he be given his job back,” said Binodi.
Devi Prasad pointed to his village home and shook his head, gesturing his desire to leave. He will not stay, not without work.
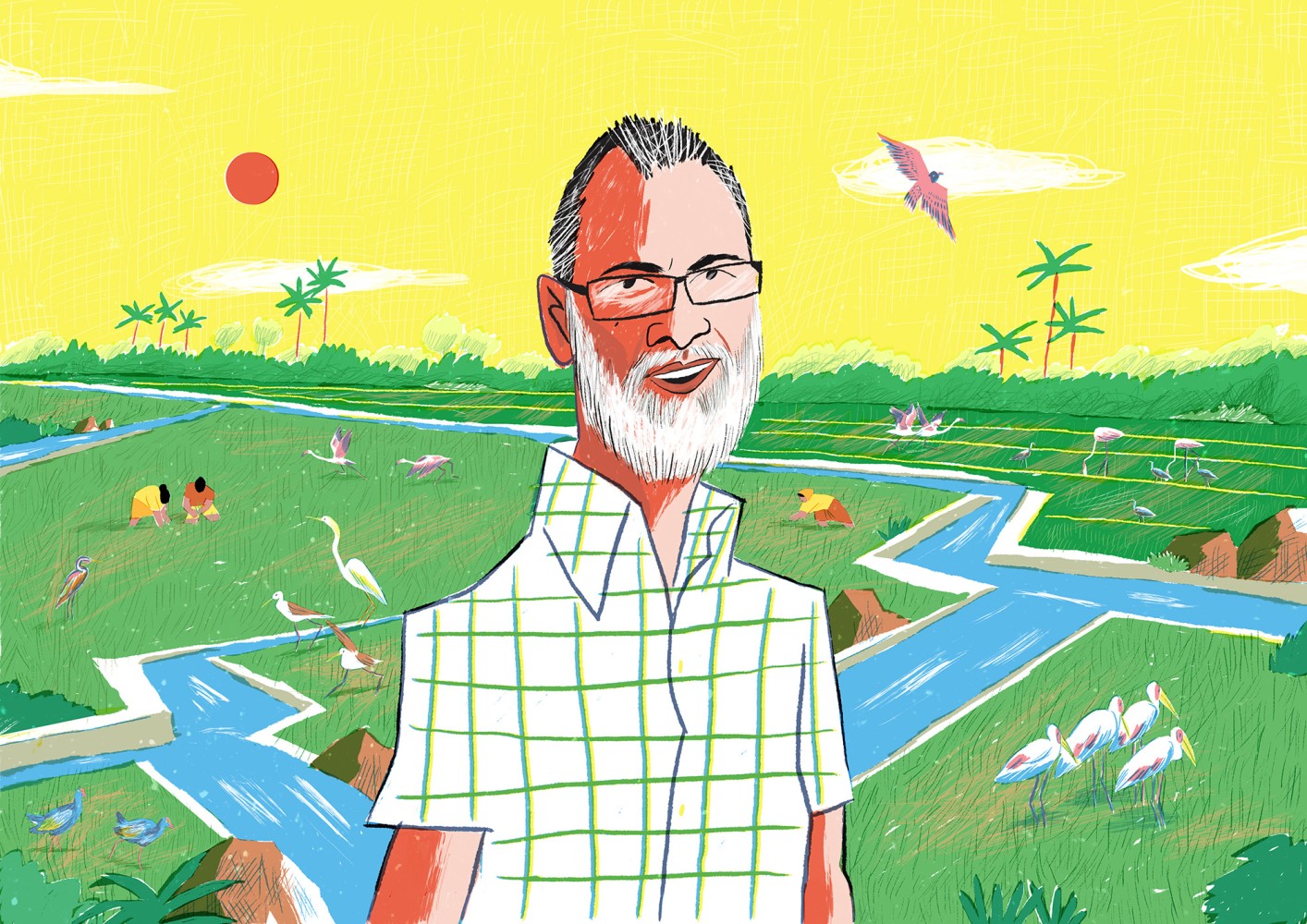
Banner image: Devi Prasad stands in the courtyard outside his home in Tikamgarh, Madhya Pradesh. Image by Simrin Sirur/Mongabay.