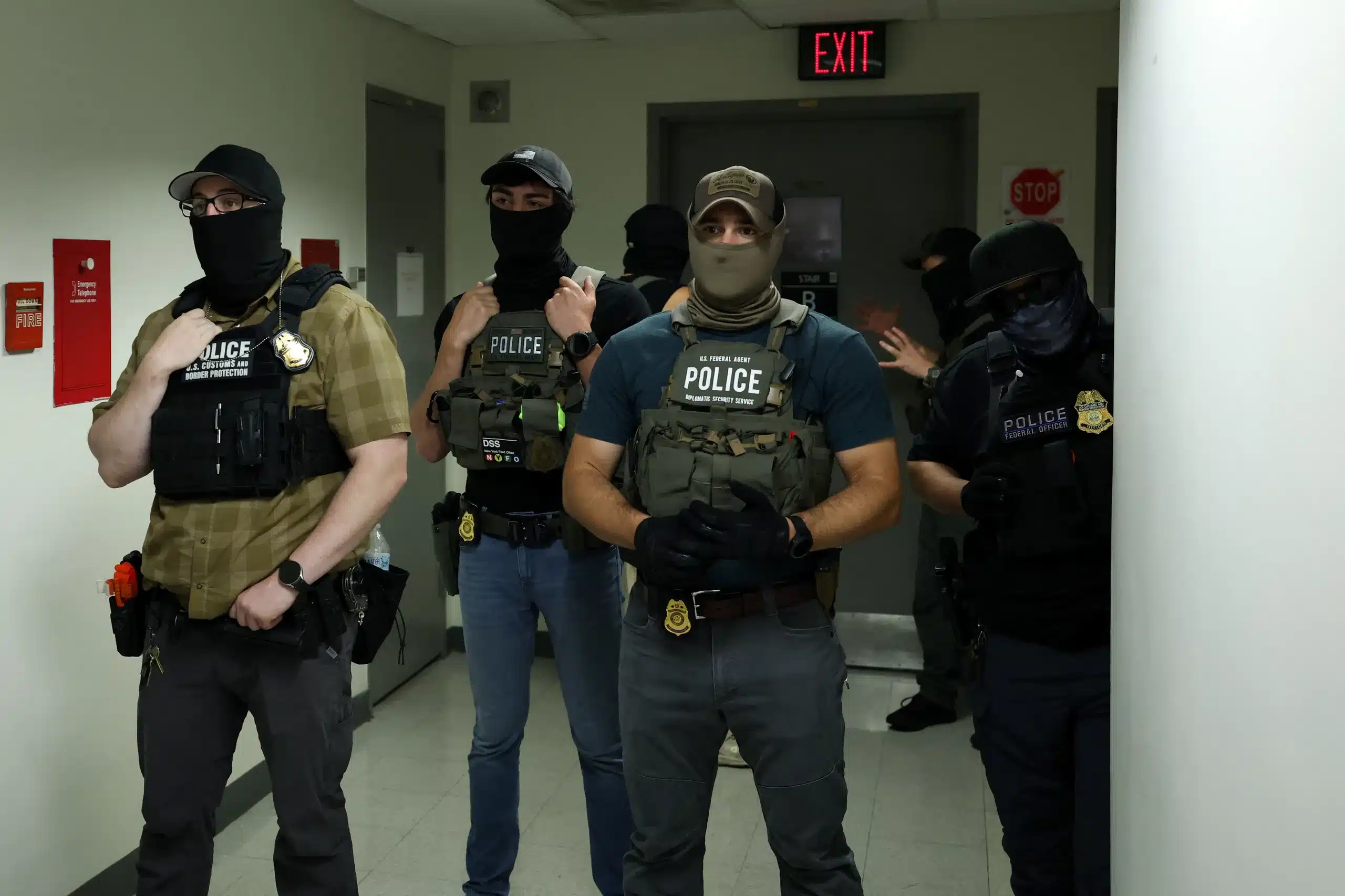
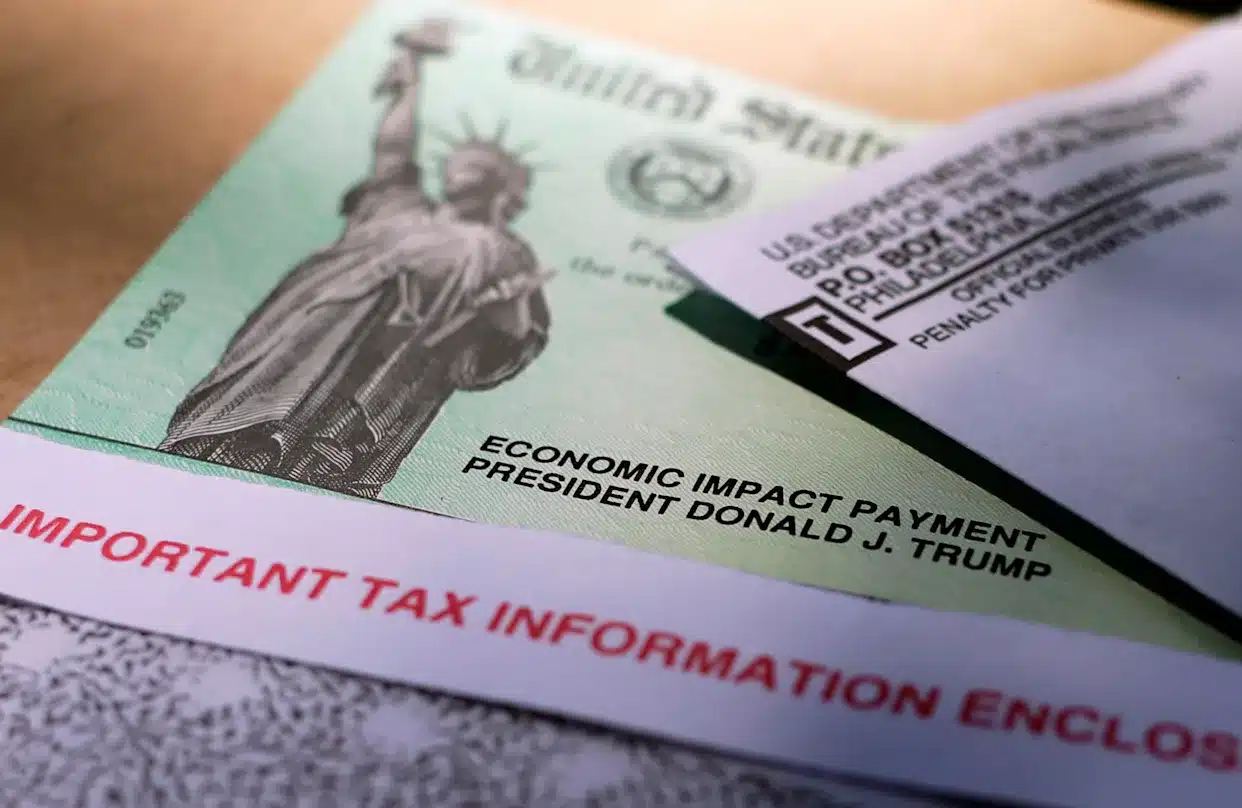
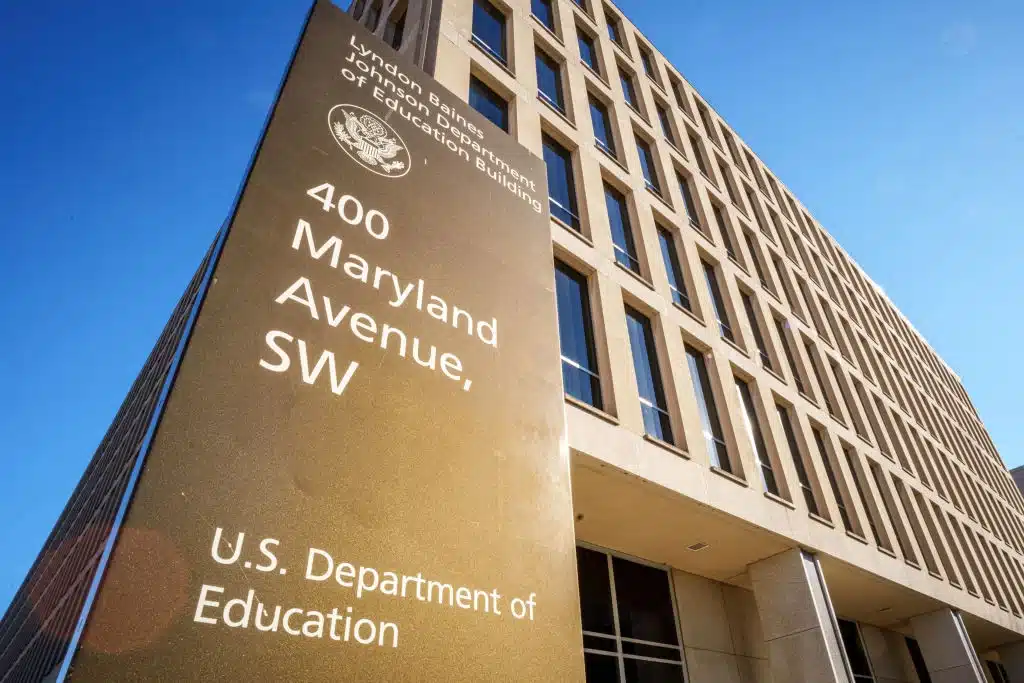
Americans are suddenly being blindsided by steep, unexpected charges at the doctor’s office – and they’re called “facility fees.”
These mysterious add-ons are popping up on bills nationwide and can go as high as $1,000 for a single visit. The surprise? These fees often hit after basic consultations lasting under 15 minutes, sparking outrage and confusion among patients everywhere.
In Minnesota, one family took their daughter for a routine stomach pain follow-up. The visit was short and the doctor’s bill came out to $201 – normal enough. But then came a $423 charge labeled “outpatient hospital services.” It caught them off guard. They’re not alone either. An Ohio man was billed $645 for facility fees after seeing an ear, nose, and throat specialist. In Boston, another patient shelled out a jaw-dropping $1,000 for a urologist visit. Even Florida residents are speaking out, with Cleveland Clinic under fire for tacking on fees of $95 to $174 for simple medical consultations.
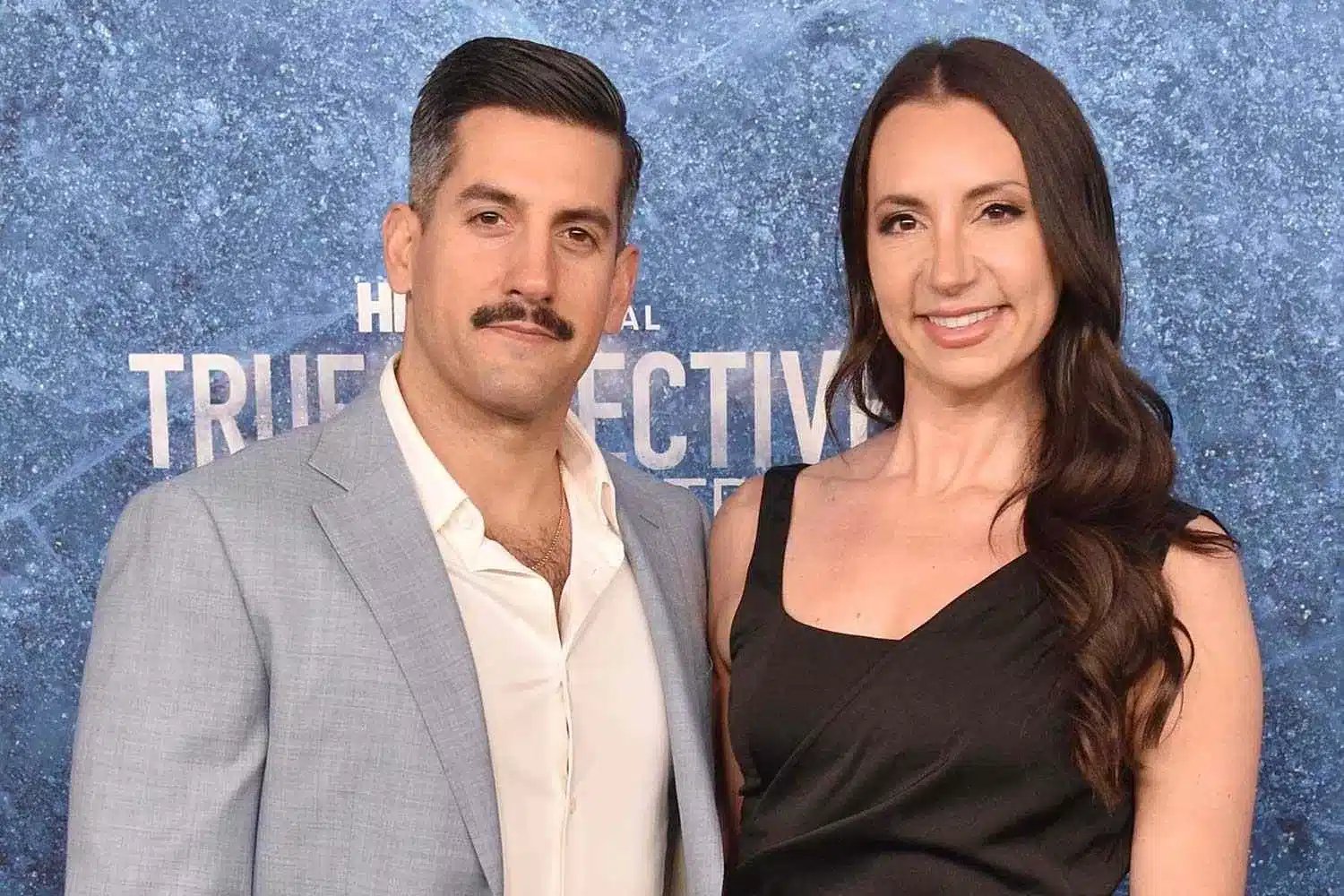
Brandy Macaluso-Owens from Port St. Lucie, Florida, told NBC News her heart dropped when she got a $174 facility fee after seeing a gastroenterologist. “I probably met with the doctor maybe as little as 15 minutes,” she said. The Cleveland Clinic responded in defense, stating the charges help cover operational costs of outpatient clinics and emergency services. They insist the practice is legal and follows healthcare industry regulations.
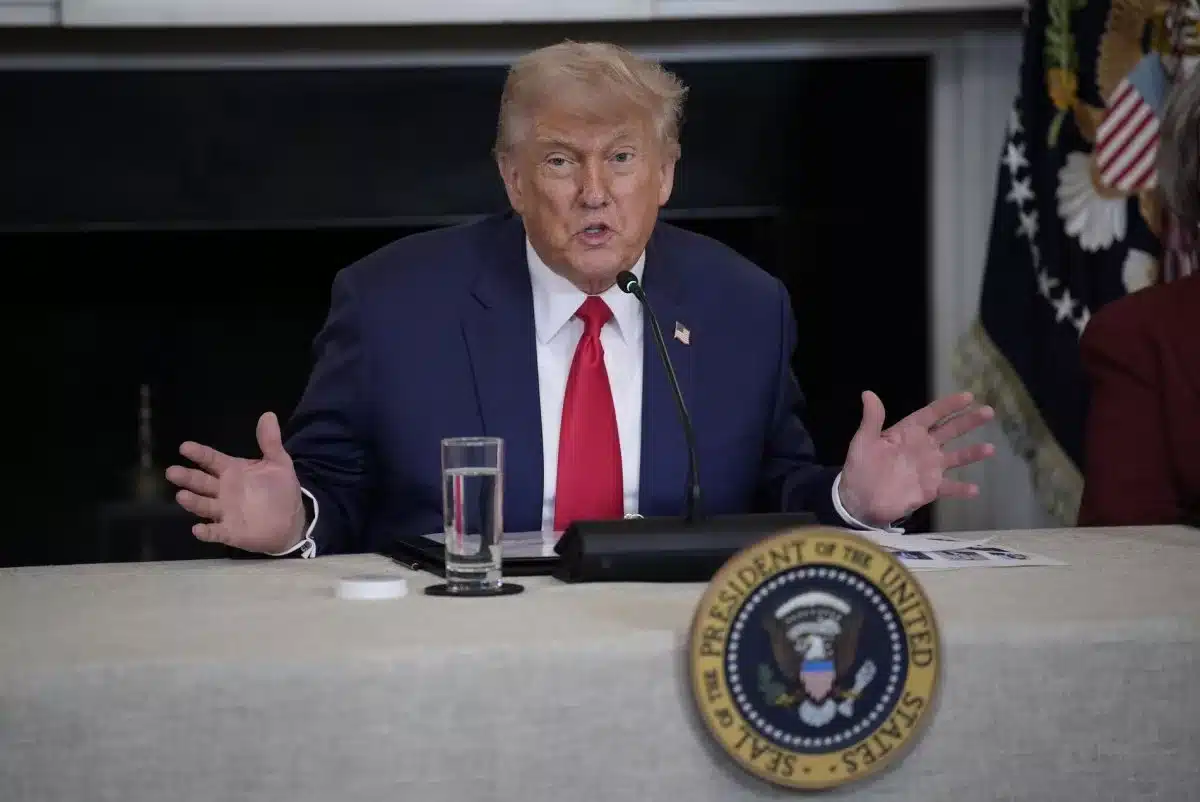
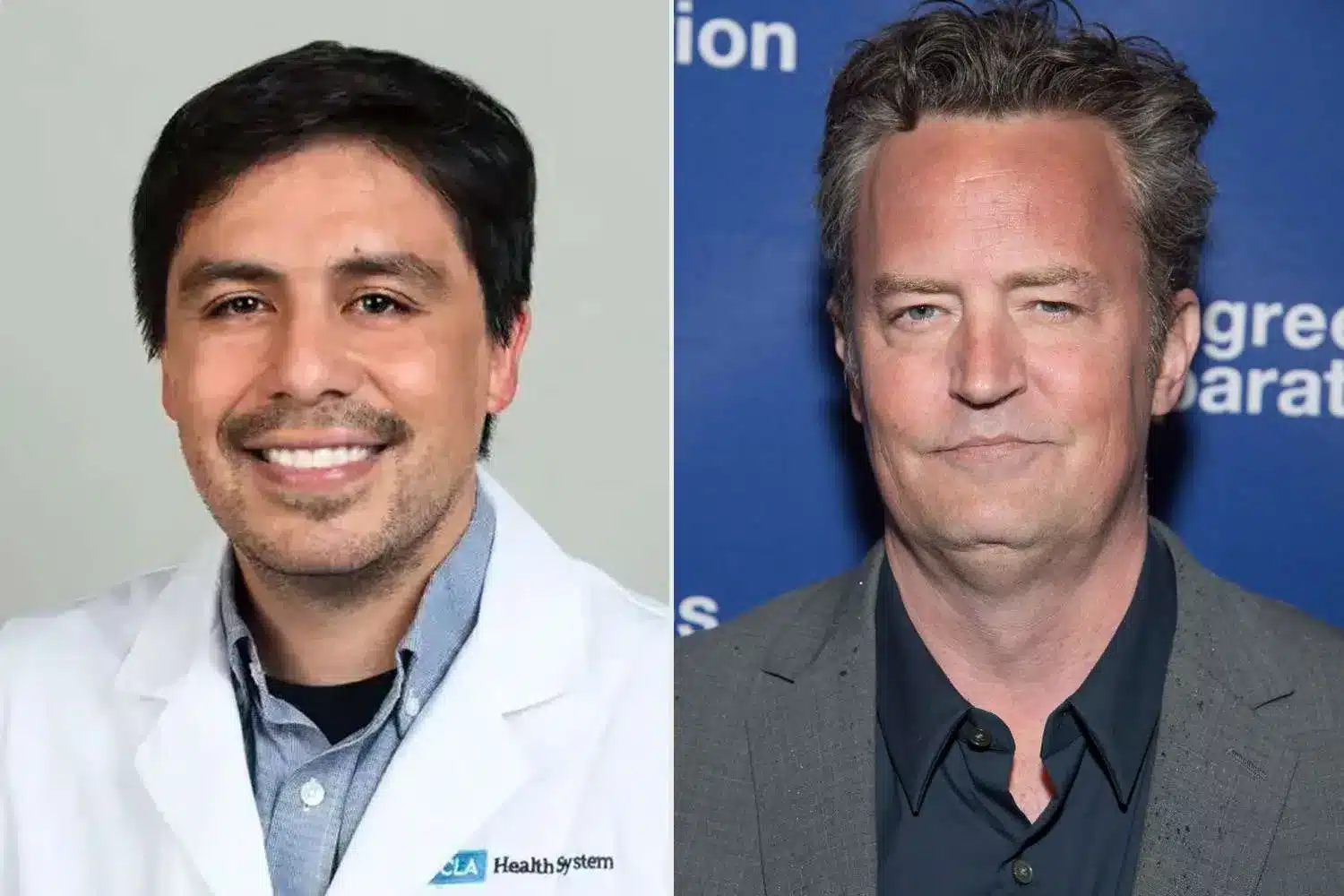
So, what exactly are these fees? According to NBC News, facility fees are becoming more common as hospitals acquire private physician practices. Many of these clinics are now classified as hospital outpatient departments, allowing them to charge fees beyond standard physician rates. Christine Monahan, a professor at Georgetown University’s Center on Health Insurance Reforms, pointed out a major issue – there’s no legal cap on how high these fees can go. “In most states and situations, there aren’t really limits,” she explained.
That means one person’s doctor visit might come with a $100 fee, while another might pay $1,000 – all for the same type of care. Insurance companies argue these charges inflate healthcare costs without adding any real value. The American Hospital Association, on the other hand, says insurers should be covering facility fees in full. This tug-of-war leaves patients stuck in the middle.
So what can people do if they’re hit with one of these charges? Healthcare experts suggest asking for a full estimate before your appointment – and don’t forget to ask if facility fees apply. If you’ve already been billed, contact the provider’s billing department to request a breakdown of charges. You should also call your insurance provider and check if they can cover the fee or help reduce your out-of-pocket cost. Patricia Kelmar, senior director at the US Public Interest Research Group, said providers may waive or lower the fee if you can’t afford it.
These fees aren’t just hitting hospitals either. Restaurants have also come under fire lately for similar billing tactics. One breakfast chain sparked backlash for adding a 50-cent fee to a menu item across all its 2,000 locations. Another restaurant faced boycott threats after an 18% “living wage fee” appeared on receipts.
But when it comes to medical care, the stakes are much higher. With insurance often covering less and fees growing more unpredictable, the average American is left trying to decode bills that look more like puzzles than invoices. Facility fees are fast becoming the healthcare system’s most unpopular surprise, and until regulations catch up, consumers are stuck asking the same question: what exactly are we paying for?