The Centers for Medicare and Medicaid Services (CMS) is getting ready to implement a pilot program that will employ artificial intelligence in determining if some medical treatments are worthy of coverage.
The initiative, scheduled to launch next year, is intended to reduce fraud, waste, and abuse in the system, say officials. However, patient advocates and health professionals are sounding alarms that the strategy may cut into seniors’ access to services.
The program will initially roll out in six states: Ohio, Oklahoma, Arizona, New Jersey, Texas, and Washington. It only affects traditional Medicare, the government-run health insurance program that insures more than 30 million Americans age 65 and older, along with individuals with some disabilities.
Under the program, certain medical treatments will need pre-authorization to receive treatment before patients can go through it. They include treatments like steroid injections, back surgeries, and skin substitutes – treatments that government officials say could be overused and cost billions of taxpayer dollars annually in unnecessary expenses.
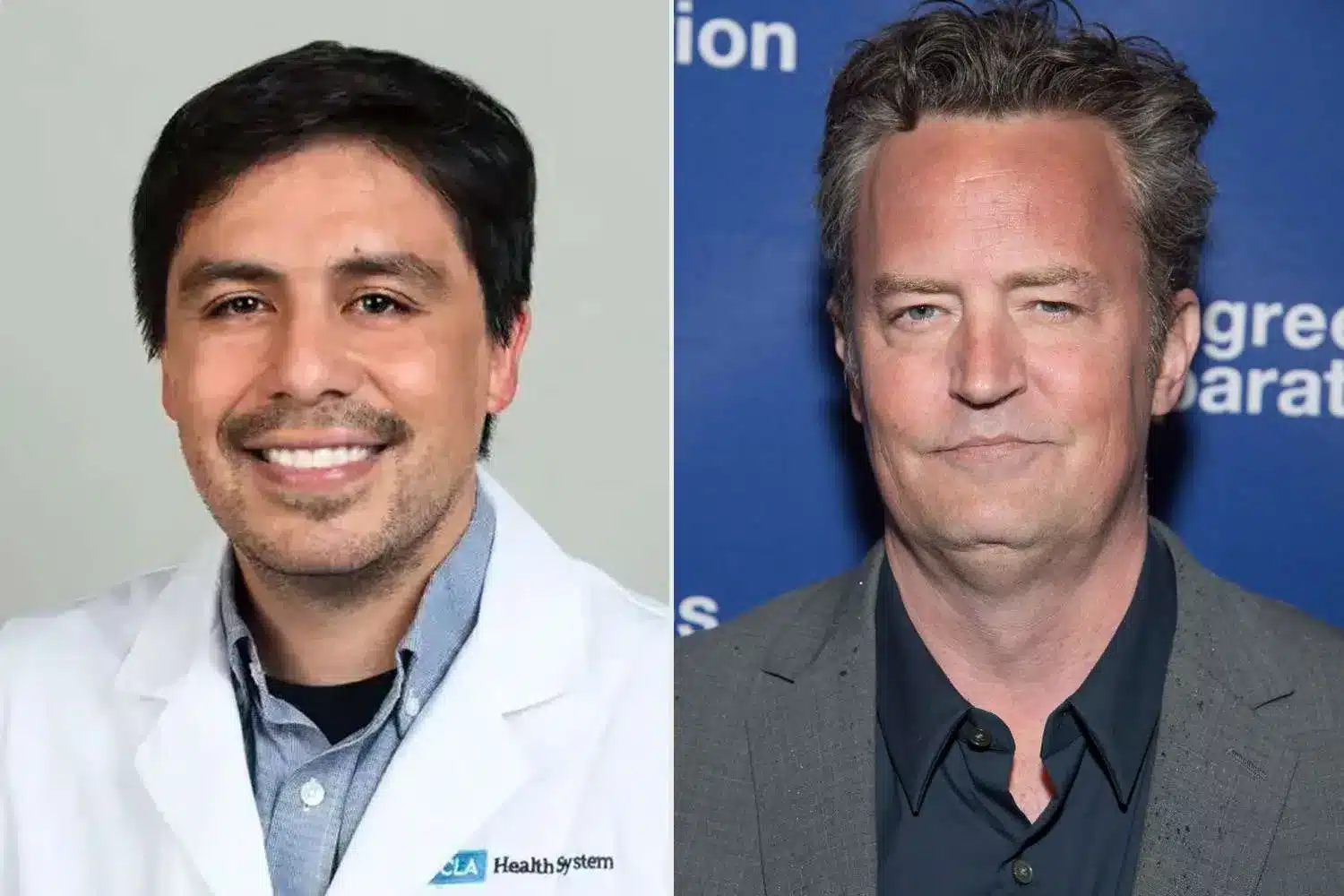
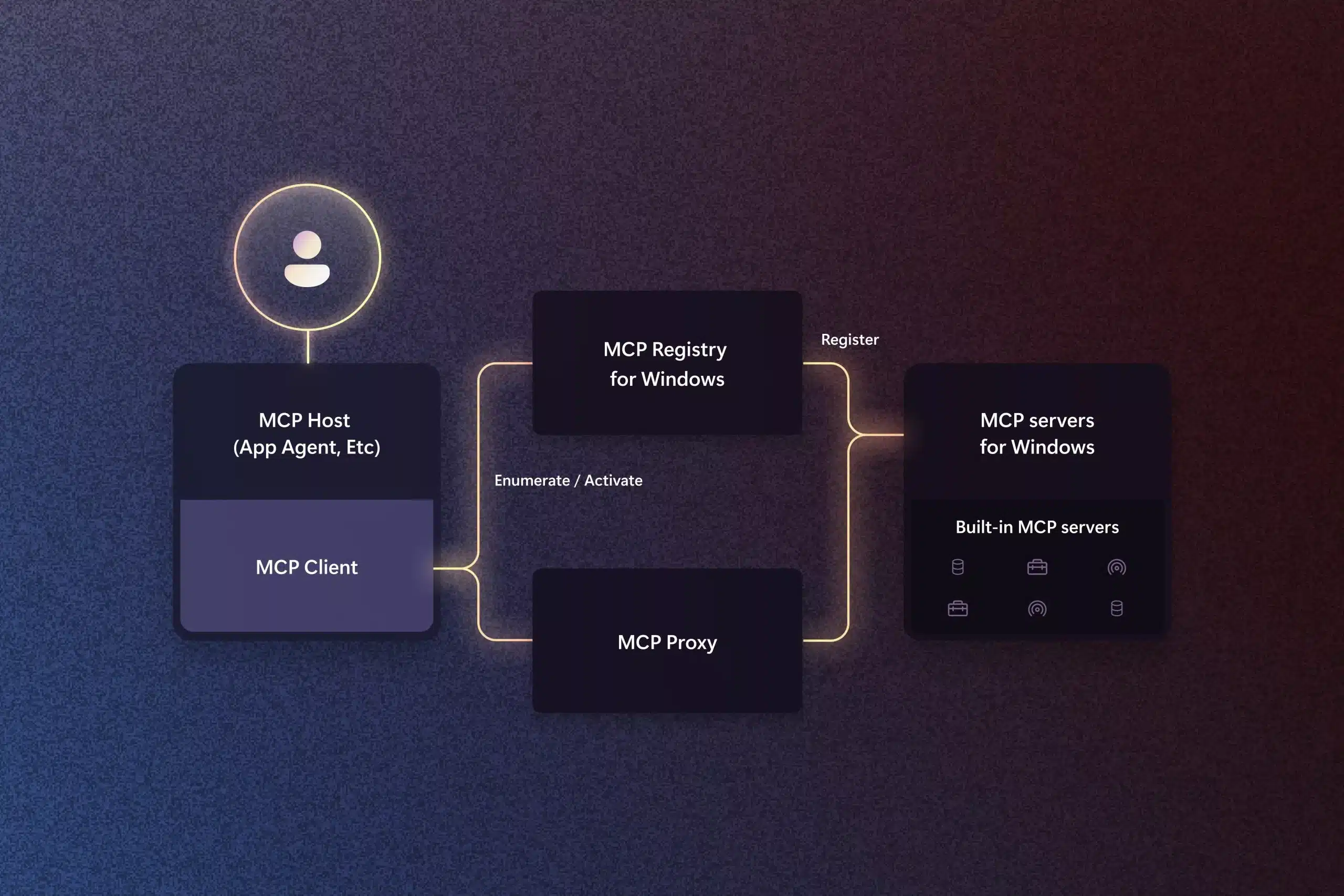
What has generated the most controversy, however, is under what terms these decisions will be made. Rather than being made solely by physicians and human reviewers, CMS has outsourced approvals and denials to private AI firms. Critics say this gives companies a financial incentive to deny requests, as they are said to be paid per denial. That, experts say, could lead to patients being denied access to treatments that they are legally allowed to receive.
If benefits are denied, patients may be forced to pay out of their own pockets unless they appeal. Physicians are urging patients to remain informed about their rights, carefully investigate their choices, and not shy away from contesting denials through the appeals channel.
Other experts fear that the increased red tape will discourage conventional Medicare from being as popular as Medicare Advantage plans, since the latter already use prior authorization for numerous services. Ironically, Medicare Advantage tends to cost the federal government more per participant, so the program might divert spending without realizing actual savings.
Another worry is that patients could receive the treatments that are easiest to approve, not necessarily the most appropriate to their health requirements. The secrecy regarding how the AI companies will be assessing cases has already generated criticism from some politicians and doctors, who say that the system threatens to put efficiency ahead of patient welfare.
The CMS has indicated the pilot program will be under tight scrutiny to assess its impact, but in the meantime, the controversy surrounding AI in medicine – and in Medicare – is only likely to increase.