- Global studies highlight the potential negative impacts of climate change on people living with diabetes.
- Despite India’s staggering count of people with diabetes, a lack of data on the effect of climate change on the condition is concerning.
- Apart from data generation, education and awareness among patients are key in managing the disease during extreme weather events.
Mumbai-based registered dietician and diabetes educator Shilpa Joshi faces a new conundrum. For more than two decades, she has been helping people living with diabetes navigate their diet and lifestyles as they manage the disease. However, in recent times, Joshi’s patients are approaching her with challenges that are beyond the dietician’s purview.
“It is raining in Mumbai and Pune now. In May, we experienced heavy rains and floods, and in March, people were suffering from heat exhaustion. With so many changes, it is difficult for patients to adhere to the diet and lifestyle protocols we recommend. Unseasonal rains have increased the price of most vegetables, and between the rains and the heat, physical activities, like walking, have become challenging. Not everyone can afford to go to gyms,” shares Joshi.
The day-to-day challenges outlined by Joshi provide a brief window into the life of a person living with diabetes in India under the shadow of climate change. According to a 2024 study published in The Lancet, India is home to 212 million people suffering from the disease, the highest in the world. Further, there has also been a marked increase in the incidence of diabetes. Between 1990 and 2021, the prevalence of diabetes in India has gone up from 162.74 people to 264.53 people per 100,000 population. In the same period, mortality from the disease has also increased from 23.09 to 31.12 per 100,000 population.
Globally, several studies have examined the links between climate change and diabetes, however data from the Indian subcontinent is lacking. A 2017 U.S.-based study showed that diabetes incidence increased by 0.314 per 1000 people for every 1°C rise in temperature. A 2019 study from Brazil showed that a 5°C rise in daily mean temperatures led to a 6% increase in diabetes-related hospital admissions, primarily among the elderly. Similarly, a recent Kuwait-based study also found that hot days (>33°C) contributed to an excess of 282 diabetic admissions annually.

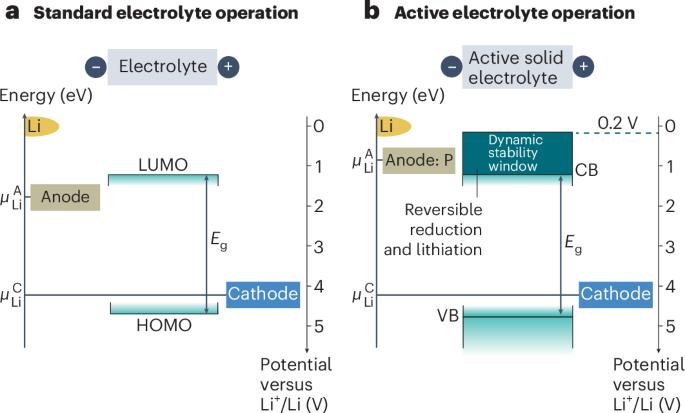
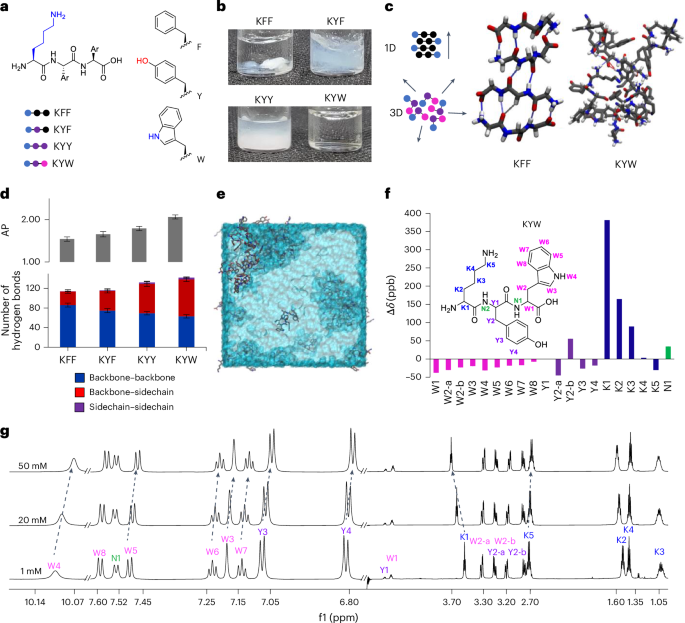
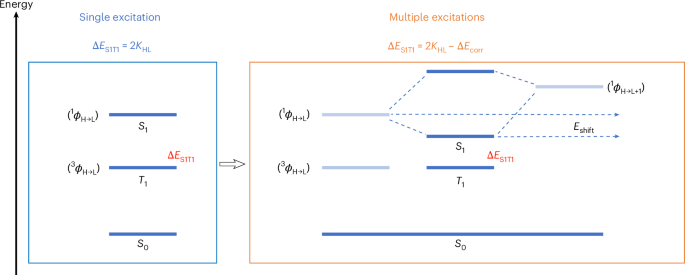
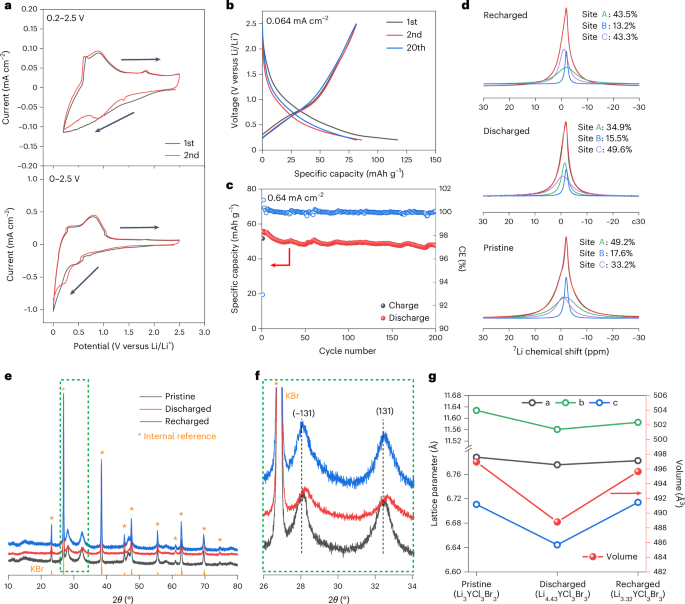
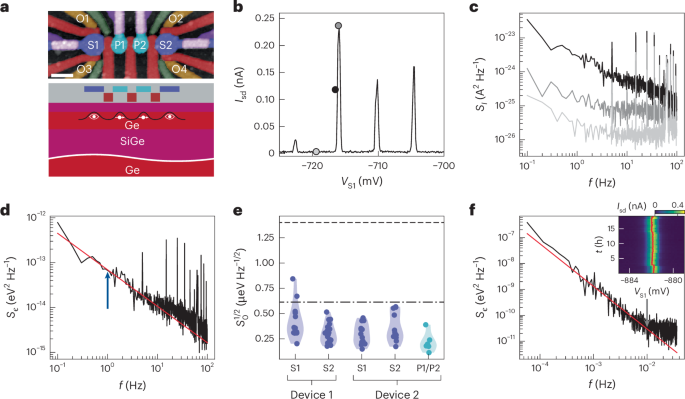
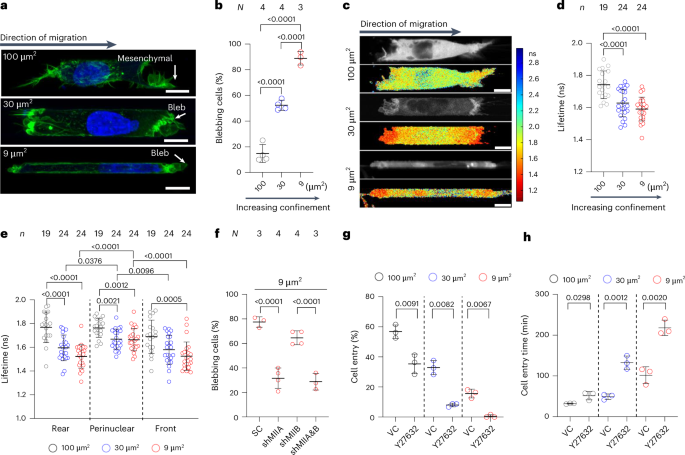
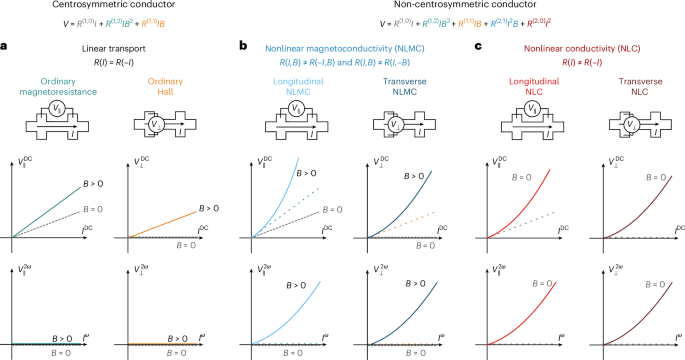
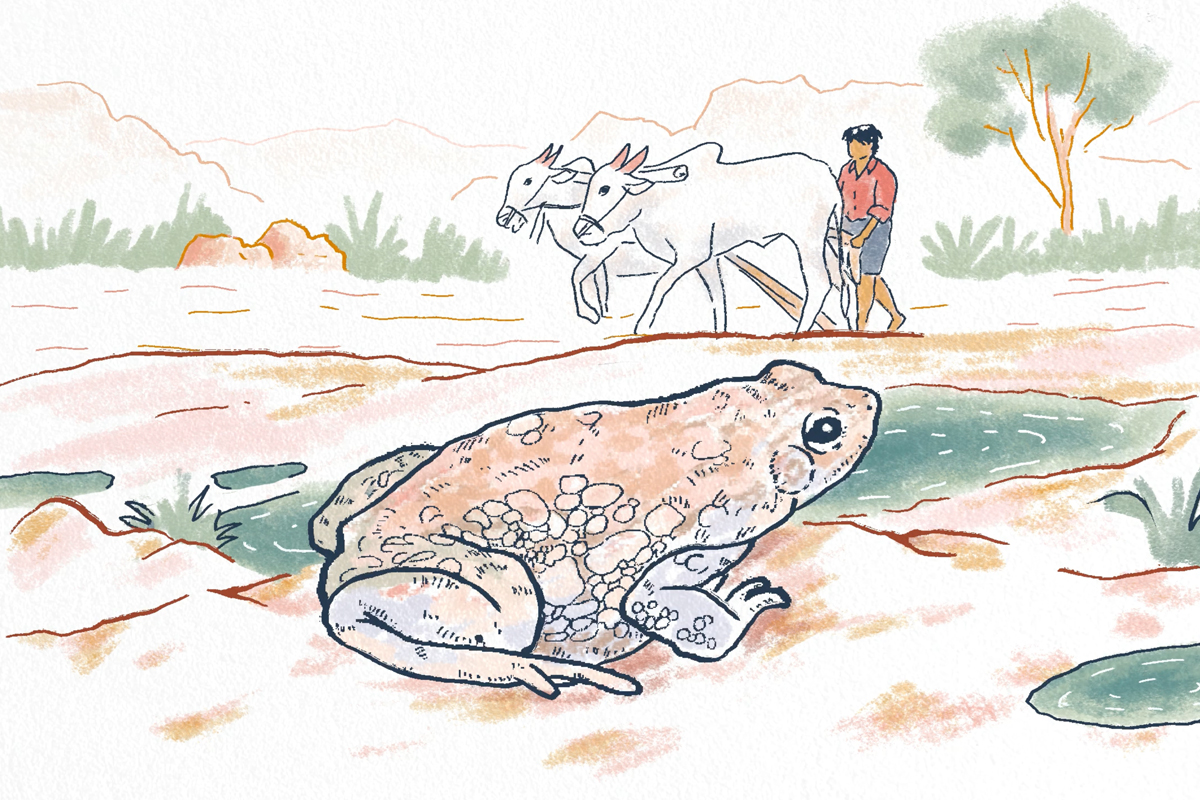
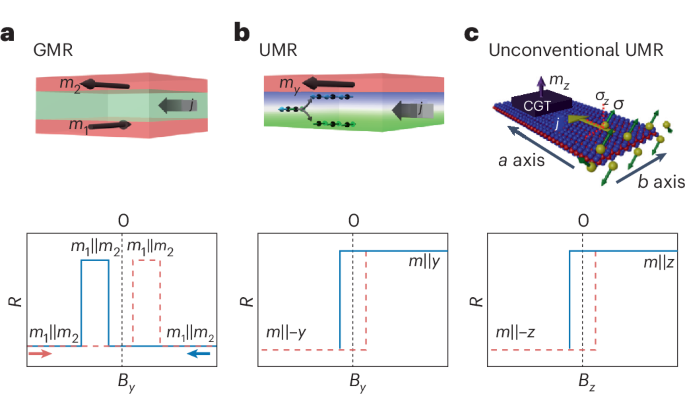
Table: Summary of global studies that examine the links between diabetes and climate change
How does climate change impact diabetes?
Among the most common non-communicable diseases in the world, diabetes or diabetes mellitus, refers to a group of metabolic disorders characterised by high blood glucose levels or hyperglycaemia. The disease is broadly classified into type 1 and type 2 diabetes, denoting inadequate insulin production (type 1) or a combination of inadequate production and poor response to the produced insulin (type 2). Other categories also include prediabetes, where individuals are at a high risk of developing the disease, and gestational diabetes, marked by the presence of the disease during pregnancy.
Existing research indicates that climate change can have varying impacts on people living with the disease. In a review article, Ratter-Rieck et al. show that extreme heat can increase the incidence of the disease. The article explains that it also affects the patient’s response to heat stress due to impaired blood flow in the skin and abnormal sweating. Some studies mentioned in the review article point to increased hospital admissions, both in extreme heat and cold conditions, and additional impacts due to comorbidities as a result of kidney and cardiovascular issues.
Apart from temperature-related impacts, studies show that extreme weather events can also cause long-term disruptions in the patient’s health and impair glycaemic control, while increasing the risks for related complications.
Researchers now also warn that climate change can increase the incidence of infections globally. Fuelled by changing temperatures, rainfall patterns, as well as changes in animal migration patterns and coastal water temperatures, experts caution that physicians must be prepared for an altered landscape where infections will be on the rise along with the emergence of new ones.
This is particularly important for people living with diabetes, as the disease makes them more susceptible to infections. Diabetes is a risk factor for infectious diseases such as encephalitis, chikungunya, West Nile virus and dengue, and therefore, the impacts of climate change on disease risks of people living with diabetes warrants a separate focus.

Lack of data hinders devising control strategies
While existing research shows that climate change can further complicate the pathophysiology of diabetes and its management in patients, significant gaps exist in our understanding of these interconnections, explains a review article by researchers from the US, UK, India and South Africa.
Based on data from 73 peer-reviewed human studies, the article shows that the majority of the observations exists from the North American and Caribbean regions. The researchers did not find relevant studies from India in their review and noted that most of the studies focused on high-income countries.
A 2023 study examining the links between air pollution and diabetes in two Indian cities, Chennai and Delhi, shows that both short and medium-term exposure to airborne particulate matter less than 2.5 micrometres in diameter, increases fasting plasma glucose levels and glycated haemoglobin (a measure of long-term blood sugar control). The study also shows that long-term exposure to air pollution increases the risk of developing the disease.
Commenting on the lack of observations from India, Siddhartha Mandal, lead author of the study and senior research scientist at Ashoka University, explains that epidemiological studies of this nature are sparse in the country not just for diabetes, but for other conditions as well.
With air pollution, for example, Mandal explains that lack of monitoring data hindered assessing exposure at the ambient level, and recent developments in satellite-based models have aided in reducing some of this gap.
“Climate change by itself encompasses air pollution, and it will have other systemic issues as well, such as changes in food and agricultural patterns. A one-degree change in temperature can set in motion several factors that may ultimately lead to the prevalence of diabetes. To study the combined effects of all these influences is a massive challenge. It is crucial to have quality health data to understand the impacts of these exposures and its outcomes,” explains Mandal.
While there is some increase in awareness on the impacts of air pollution and climate change on human health, it will take a while for the existing evidence to be collated for policy-level interventions in India, explains Mandal. “But, the efforts are ongoing,” he says.

An evolving landscape
In April 2025, the International Diabetes Federation (IDF), launched a working group to develop treatment recommendations and diagnostic criteria for a newly recognised category of diabetes called type 5 or Malnutrition Modulated Diabetes Mellitus (MMDM). With chronic undernutrition during the early stages of life being a leading cause for this category, IDF states that the disease is prevalent among teens and young adults in low and middle-income countries (LMICs).
Dr. Nihal Thomas, senior professor of endocrinology at Christian Medical College (CMC), Vellore, and co-chair of the working group, explains that type 5 diabetes was first reported in 1955 in Jamaica and was later classified in 1985 by the World Health Organisation. However, lack of physiological evidence and misdiagnosis as type 1 or 2 led to the classification being removed in 1999.
He adds that the renewed interest in type 5 diabetes is especially crucial for India. In a study of low birth rates among 44 LMICs, India had the third highest prevalence of low birth-weight births. The Global Hunger Index (GHI) 2024 also states that 13.7% of India’s population is undernourished, and 35.5% of children in the country under the age of five are stunted as a result of chronic undernutrition. “If there is low birth weight followed by undernutrition during the developmental years, it is a double hit, increasing one’s risk for type 5 diabetes,” explains Dr Thomas. He adds that while other metabolic processes also contribute to the disorder, the role of dietary factors is of significance here and the impacts of climate change in this regard needs further investigation.
Several studies have highlighted the fact that climate change not only reduces agricultural productivity; it also diminishes the nutritional value of crops, thereby contributing to food insecurity and undernutrition. Dr Thomas adds that looking at the links between climate change, undernutrition and the prevalence of diabetes will require more representative data at scale, which is challenging to obtain. Furthermore, he also emphasises the need to understand these influences in urban and rural settings as they will lead to differences in the way the disease develops and progresses.
“While it is important to look at the links between diabetes and climate change, it is not that straightforward. If you list all the risk factors for type 2 diabetes, for example, you will find that every factor will be a confounder when you study the others. Diet assessments will also need to consider physical activity, and conducting accurate physical activity evaluations are very difficult. These studies need to be well-planned,” he adds.
Adding to the discussion, Charles E. Leonard, associate professor of epidemiology at the Perelman School of Medicine in Philadelphia, emphasises the need for granular data so personalised diabetes management can factor in the individual’s environment. “Focus on extreme temperatures has largely been limited to curbing excess physical activity and issues with storing insulin. So far, there has been very little specific focus on how unusually high or low ambient temperatures, for example, could impact diabetes treatment decisions,” he explains.
Apart from data generation, Leonard also emphasises the need for healthcare providers to build awareness among their patients. “Healthcare providers may wish to educate their patients on potential risks of environmental extremes — and how such events (e.g., a heatwave) in the setting of their chronic disease could place them at a disproportionate risk for harm. Furthermore, they may also consider designing personalised preparedness plans such that patients know the appropriate actions to take to manage their diabetes during extreme weather events,” he adds.
Read more: Increasing pointers to climate change indirectly impacting tuberculosis rise
Citation:
- The effect of extensive flooding in Hull on the glycaemic control of patients with diabetes. Ng et al., 2011
- Diabetes incidence and glucose intolerance prevalence increase with higher outdoor temperature. Blauw LL et. Al., 2017
- Short-term association between ambient temperature and acute myocardial infarction hospitalizations for diabetes mellitus patients: A time series study. Yu Lam et al., 2018
- Association between Heat Exposure and Hospitalization for Diabetes in Brazil during 2000-2015: A Nationwide Case-Crossover Study. Xu et al., 2019
- Higher ambient temperature is associated with worsening of HbA1c levels in a Saudi population. Alghamdi et al., 2021
- Risk Of Infections, Chronic Diseases And Mental Health Disorders After Floods By The Coastal Child Phenomenon In Displaced Populations, Piura, 2017. Loayza-Alarico et al., 2021
- Temperature and non-communicable diseases: Evidence from Indonesia’s primary health care system. Manuela Fritz, 2022
- Combined impact of heat and dust on diabetes hospitalization in Kuwait. Alahmad et al., 2024
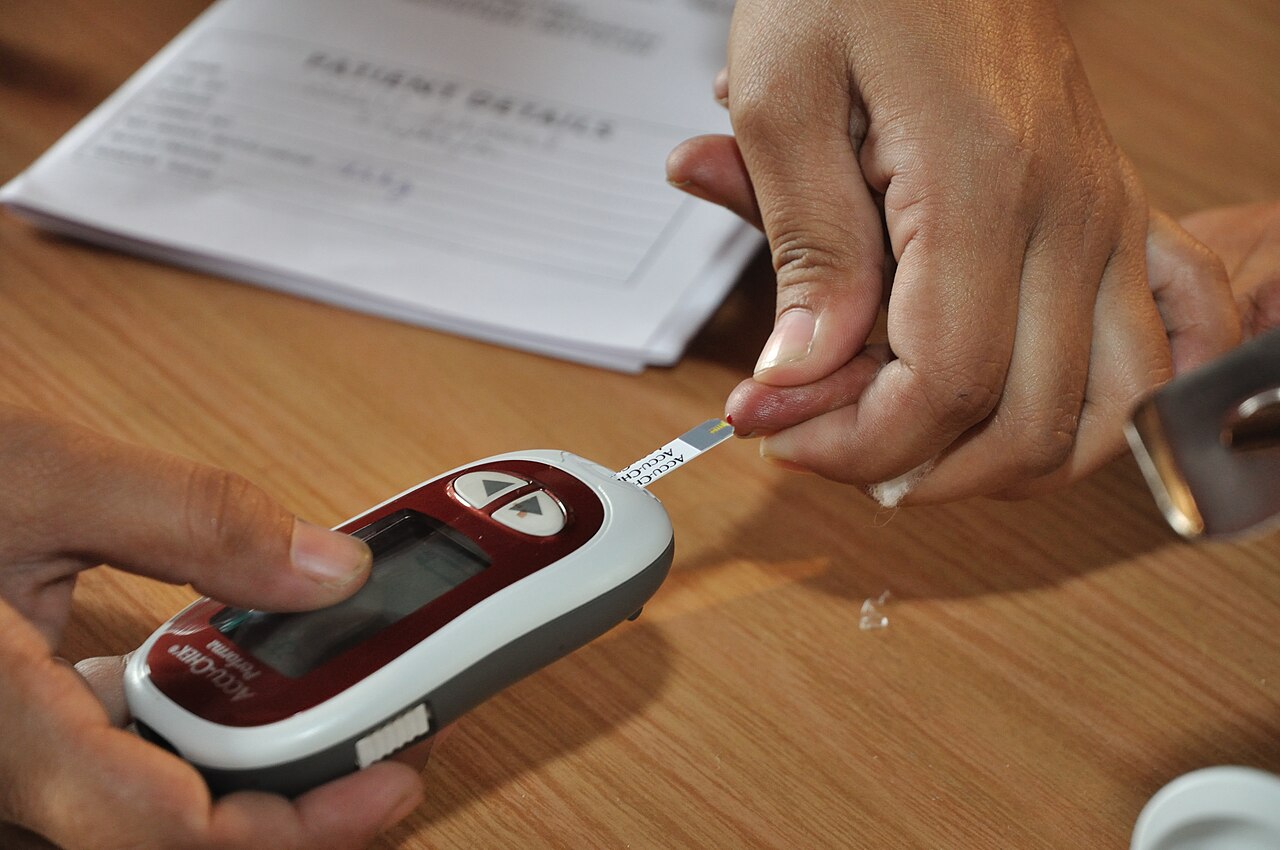
Banner image: Blood glucose testing being conducted in a clinic in Kolkata. Representative image by Biswarup Ganguly via Wikimedia Commons (CC BY 3.0).